-
UPPER GI ENDOSCOPY
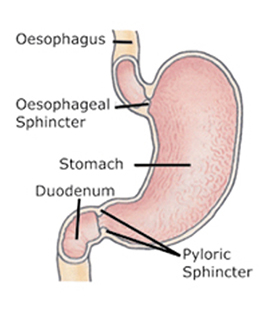
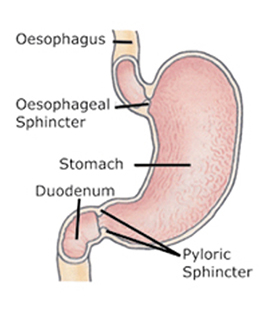
Gastroscopy, also known as a Panendoscopy, or Upper GI Endoscopy, allows the Endoscopist to examine the oesophagus, stomach and duodenum, using endoscopes, which are equipped with miniaturized, high quality video cameras. This examination will also allow the Endoscopist to take tissue samples (biopsies) for pathology testing.
This procedure is performed to investigate conditions such as:
- Ulcer Disease - Peptic Ulcer
- Difficulty in swallowing – Dysphagia
- Gastro Oesophageal Reflux disease – Acidity –GERD
- Helicobacter pylori infection
- Achalasia
- Barret's Oesophagus
- Complications of liver disease
- Dyspepsia
- Oesophageal Cancer
- Stomach Cancer
-
COLONOSCOPY
Colonoscopy allows the Endoscopist to examine the entire large intestine (colon) of a patient. A colonoscope, which is a long flexible tube equipped with a miniaturized high quality video camera at its tip, is inserted through the anus. This allows the Endoscopist to see inside the Colon, and take tissue samples (biopsies). Sometimes Colonoscopy is performed to remove polyps from the Colon.
This procedure is performed to investigate conditions such as
- Bleeding from the Rectum
- Colonic Polyps
- Causes for Constipation
- Diverticulosis
- Irritable Bowel Syndrome
- Tuberculosis of the intestines
- Crohn’s Disease
- Ulcerative Colitis
- Colon Cancer

-
ENDOSCOPIC SURGERY
Gastroscopy, also known as a Panendoscopy, or Upper GI Endoscopy, allows the Endoscopist to examine the oesophagus, stomach and duodenum, using endoscopes, which are equipped with miniaturized, high quality video cameras. This examination will also allow the Endoscopist to take tissue samples (biopsies) for pathology testing.
This procedure is performed to investigate conditions such as:
- Ulcer Disease - Peptic Ulcer
- Difficulty in swallowing – Dysphagia
- Gastro Oesophageal Reflux disease – Acidity –GERD
- Helicobacter pylori infection
- Achalasia
- Barret's Oesophagus
- Complications of liver disease
- Dyspepsia
- Oesophageal Cancer
- Stomach Cancer
-
SEDATED ENDOSCOPY PROCEDURES
Gastroscopy and Colonoscopy procedures can be performed under sedation or anaesthesia if required.
-
BRONCHOSCOPY & LARYNGOSCOPY
-
CAPSULE ENDOSCOPY
Small Bowel Capsule Endoscopy allows the Doctor to examine the three portions (duodeum, jejunum, ileum) of a patients small intestine and identify numerous pathologies present within the small intestine. It has become an important tool for evaluation of suspected diseases in the small bowel.
The endoscope is a vitamin-pill sized capsule equipped with its own camera and light source, and this is ingested. While the video capsule passes through the patient's digestive tract, images are transmitted to a data recorder worn on a waist belt. After the procedure, the Doctor will view a colour video taken from the capsule, and provide the results.
The Capsule Endoscopy can provide images of the hard to reach areas of the small intestine. The capsule is single use.
This procedure is performed to investigate conditions such as:
- Crohn’s Disease
- Coeliac Disease
- Small Bowel tumours

Preparation
Patients are required to start fasting the day before the procedure, as an empty stomach allows optimal viewing conditions. You should also inform the Doctor of any medications you take, presence of a pacemaker, previous abdominal surgery, swallowing problems or previous history of obstructions in the bowel.
After ingesting the capsule and until it is excreted, patients should not have a Magnetic Resonance Imaging (MRI) examination or be near an MRI device.
The capsule is disposable, it progresses naturally with your bowel movement and does not need to be recovered. There should not be any pain or discomfort during capsule excretion
-
BREATH TEST FOR H.PYLORI
The C14 Urea Breath Test (UBT) is a “non-invasive” diagnostic tool used to diagnose a current infection with Helicobacter pylori (H. pylori).
H. pylori are bacteria which infect the stomach lining. These bacteria have been proven to cause many conditions like duodenal and gastric ulcers, Gastric Cancer and Lymphoma.
H. pylori infection can be eradicated with antibiotics.
The Urea Breath Test is performed and processed at our Centre. The test takes a total of 20 minutes to complete. There is no discomfort experienced by patients. The result can be obtained the same day.
Patients are required to fast prior to this test with no food or drink for a minimum of 4 hours. The test procedure requires patients to swallow a capsule with water. After several minutes a sample of breath is collected. This sample is processed and the result is available the same day.
This test is a very effective test, provided the patient has not had any antibiotics in the previous 4 weeks. The patient should also avoid “acid blockers” for at least 3 weeks prior to the test.

-
ACID REFLUX COUNSELLING - GERD CLINIC
Acid Reflex Disease Testing and Evaluation Lifestyle and Nutrition Counselling to prevent Reflux Disease
-
COLON CANCER SCREENING
In the last 10 years, the incidence of colorectal cancer (CRC) has more than doubled. Initially it was thought to be not very prevalent in our country. But now, it is a frequently diagnosed condition.
There is now awareness that this Colon cancer is preventable, if it is diagnosed early.
Colon cancer most commonly develops from benign polyps which occur on the bowel wall. These polyps may increase in size and result in cancer. Polyps are thought to develop due to an unbalanced diet, smoking, excessive alcohol consumption, lack of exercise and obesity. Those at risk of developing this type of cancer include individuals with family history of Colorectal Cancer (CRC) and/or polyps, as also those with a personal history of Ulcerative Colitis, colon polyps, and other types of cancer.
The more common symptoms of CRC are rectal bleeding, abdominal pain, weight loss and changes in the bowel habits. The problem is that many polyps and early cancers do not produce any symptoms at all.

The best part is that Colorectal Cancer is preventable, and also curable, provided it is detected at an early stage. One of the best screening methods in use today is called “colonoscopy.” This procedure allows the Endoscopist to visualise the Colon, and the terminal part of the small intestine, determine the presence of polyps and/or other abnormalities, and if necessary, remove these polyps.
The world over, screening Colonoscopy for detection of polyps and Colon Cancer is mandatory from the age of 50, and is repeated every five years. In some countries the screening starts much earlier, from the age of 40, or even earlier, as in Japan. Japan has one of the best Colon Cancer screening programs, where they detect very early polyps, and prevent their progression to Cancer.
If you are 50 years of age or older, or have a family history of cancer or polyps, please consider having a screening colonoscopy. Our staff will be happy to guide you with this.
Early detection and treatment of Colon cancer is vital.
-
STRICTURE DILATATION
-
VARICES SCLEROTHERAPY
-
SIGMOIDOSCOPY
-
COLONOSCOPY POLYPECTOMY
-
OESOPHAGEAL DILATATION
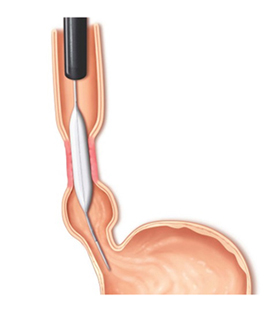
Oesophageal Dilatation is performed during Upper GI endoscopy, to open up a narrowing (stricture) of the food pipe ( oesophagus).
Endoscopic Balloons are devices which are passed through the endoscope, into the narrowing in the food pipe, and expanded to widen the narrowed segment. This may be performed also by using a fine guide wire which is passed through the endoscope down the foodpipe, The dilator then slides along the guiding wire allowing the Gastroenterologist to expand the blocked foodpipe. This procedure is also performed using image intensifier guidance.
This procedure is useful for treating numerous Upper stricture-producing GI conditions such as:
- Hiatus Hernia with narrowing
- Barrett’s Oesophagus
- Gastro Oesophageal Reflux Disease (GORD)
- Oesophageal Cancer
- Dysphagia due to narrowing
- Achalasia

Disable Preloader